Medical treatment has made tremendous progress in recent years, with the emergence of groundbreaking technologies such as robotic surgery. These innovations have been made possible by the collaborative efforts of researchers from various engineering fields, such as informatics, electrical, mechanical, and other specialized disciplines. Even before “medical-engineering collaboration” became a buzzword, Chiba University had established many laboratories engaged in future medical technologies with a focus on medical-engineering education and research. In a recent interview, Professor Toshiya Nakaguchi and two Chiba University Ph.D. students shared their insights on the latest advancements that are poised to address real-world healthcare challenges.
Robust and cohesive medical-engineering collaboration: the role of Center for Frontier Medical Engineering (CFME)
Dr. Nakaguchi, can you tell us about the CFME, where you perform your research?
Medical-engineering collaboration is one of the most-watched fields today, represented by the announcement in October 2022 of the merger between Tokyo Medical & Dental University and the Tokyo Institute of Technology. So, what characterizes such “medical-engineering” collaborations? It entails cooperation among three groups: 1. Medical professionals and institutions, 2. manufacturers of medical devices and equipment, and 3. researchers in various engineering fields who can develop new technologies. The cooperation and coordination of these three groups foster the creation of breakthrough medical devices and equipment.
Chiba University’s Center for Frontier Medical Engineering (CFME) was established in 2003. Over its 20-year history, the CFME has engaged in extensive dialogues and partnerships with doctors and joint research companies worldwide, including in Japan. These collaborations have led to numerous research achievements, making CFME a rare and valuable research institution in the country.
Despite the exciting potential of medical-engineering collaboration, it’s important to recognize that not every promising idea can be easily put into practice. In fact, this is a particularly challenging and intricate field, in part because medical professionals and engineers often have completely different ways of thinking and communication styles to express their ideas. At the CFME, we have built up a wealth of experiences and expertise that allows us to listen carefully to each party’s perspectives and ideas. Through this, we have earned the trust and respect of all stakeholders involved, paving the way for fruitful and productive relationships. Ultimately, these experiences give the CFME major advantages in navigating the complexities of medical-engineering collaborations.
So, the CFME has established a strong base for medical-engineering collaborations. Can you explain how you typically initiate your project?
First, we sit down with the visitors to determine what their worries are, and where the problems lie. We encourage them to explain their technical terms and unclear points in everyday language, so we can get to the core of the problem. Once we have a clear understanding of the real issues, we dive deeply to find the optimal solutions and suggest proposals accordingly. Our goal is to deliver tailored solutions that address the root cause of the problem.
If we determine that we require specialized knowledge and technologies from other professors, we seek out their participation in our projects. We at the CFME have extreme flexibility in our lateral networks, allowing us to pursue cross-sectional joint projects that link various research labs. In addition, the Center has three full-time professors who are also medical doctors, an unusual combination for this type of institution in Japan. Heir firsthand experience and candid insights as practicing medical professionals enable us to make rapid progress in our research. Truly, we feel fortunate to have such a talented staff and supportive environment at the CFME.
Medical imaging with projection mapping on patients’ body

Dr. Nakaguchi, your field of specialization is imaging technology. Could you please tell us more about this?
Simply stated, we use projection mapping to create an internal map of a patient’s body, which we then project onto the surface of the body. This allows us to perform laparoscopy, a far less invasive alternative to conventional abdominal surgery, with a reduced burden on the patient. Yet, laparoscopy involves a very unnatural posture, as the surgeon must perform procedures while watching the monitor located above. Not only is this an extra load on the eyes and shoulders of the surgeon, but it is also taxing for the brain, as the surgeon must follow the monitor while transposing the image onto the actual surgical field being worked on. This is, thus, a surgical technique that demands additional skills, concentration, and precision.
As a solution, we have developed a navigation system for laparoscopic surgery that uses projection-based augmented reality. With this system, the surgeon can “see” the inside of the body cavity as the surgery progresses, as the “pop-out” projection onto the body surface enables an intuitive and accurate grasp of what is occurring inside the patient.

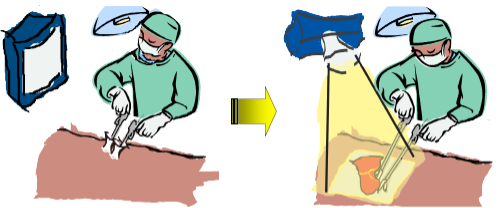
Right (laparoscopy with the new system): With a projection of a real-time image of the surgical field onto the body, the surgeon has an intuitive understanding of the surgical field. This greatly reduces the burdens inherent to conventional laparoscopy.
Aside from its use in creating impressive visual displays for events, projection mapping technology is also being utilized in the medical field. What other technologies are you involved with?
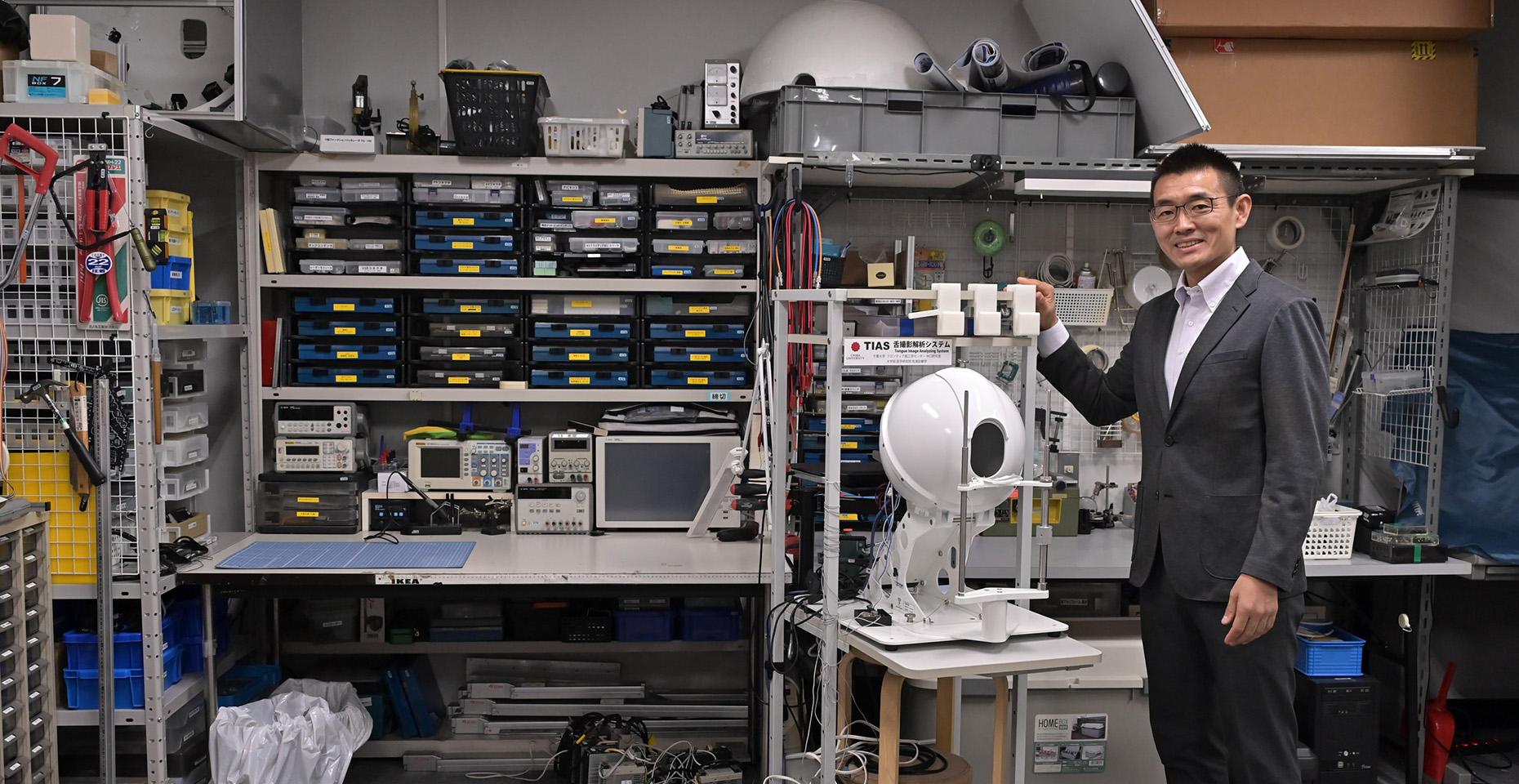
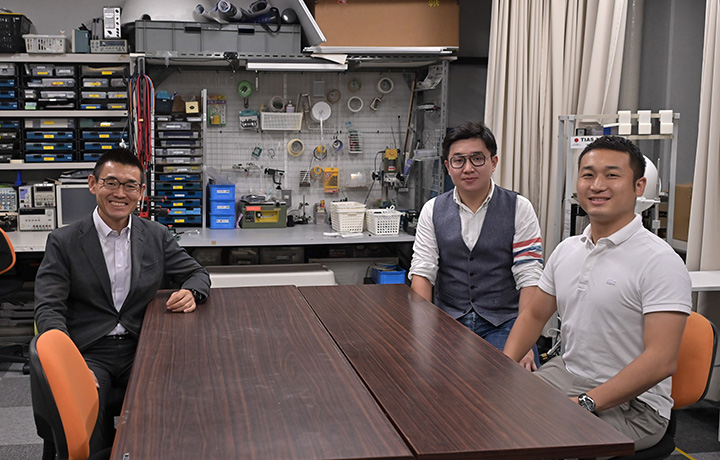
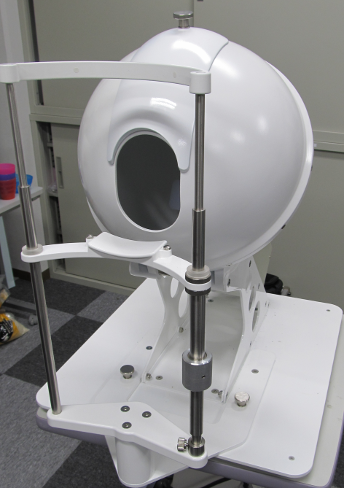
My team is currently working on developing a technology that can support tongue diagnosis. The tongue is often called the “mirror of the whole body,” and changes in its color or shape can indicate changes in a person’s physical condition. If these changes can be detected early on, tongue diagnosis could be a valuable tool in preventing illnesses. However, up until now, there hasn’t been a reliable way to accurately image the tongue and its current state.
That’s where our Tongue Image Analyzing System (TIAS) comes in. It’s a specialized system that uses “integrating sphere lighting” technology to create clear and precise recordings of the surface of the tongue. By sharing this device with researchers both in Japan and internationally, we’ve collected a significant amount of data on tongue states. Our ultimate goal is to develop a system that can support tongue diagnosis using artificial intelligence (AI) technologies, which could help prevent illnesses before they become more serious.
Embracing Patient-Centric Healthcare: Communication Takes the Spotlight
So, you are pursuing realistic training systems.
The current training involves simulations with training mannequins or healthy individuals, falling short of capturing the intensity of real-life medical situations. We thus developed EARS, a simulator that enables a doctor/trainee to find abnormalities in biological sounds (such as heartbeats and breathing) while engaging in consultation with a patient. EARS is a simple yet realistic simulator that replaces healthy biological sounds with abnormal ones, providing a low-cost way to achieve realistic training where a doctor/trainee can distinguish abnormal sounds while speaking with actual human patients.
Dr. Nakaguchi, you really place a high value on dialogue and communication.
I personally think that there are two main categories of skills for medical personnel: technical and non-technical. Communication skills fall into the latter category. We are in an era where patients have the autonomy to choose their own treatment approach, which requires doctors to provide thorough explanations to their patients.
Additionally, the risk of medical malpractice litigation is significant, and inadequate communication between doctors and patients is a common cause of such litigation. Therefore, our goal is to create diagnostic and other systems with rich resources for doctor-patient communication, as well as to reduce the burden on doctors.
Training next-generation researchers in medical engineering
We heard that you are putting a lot of effort into the education of future leaders in next-gen medical engineering.
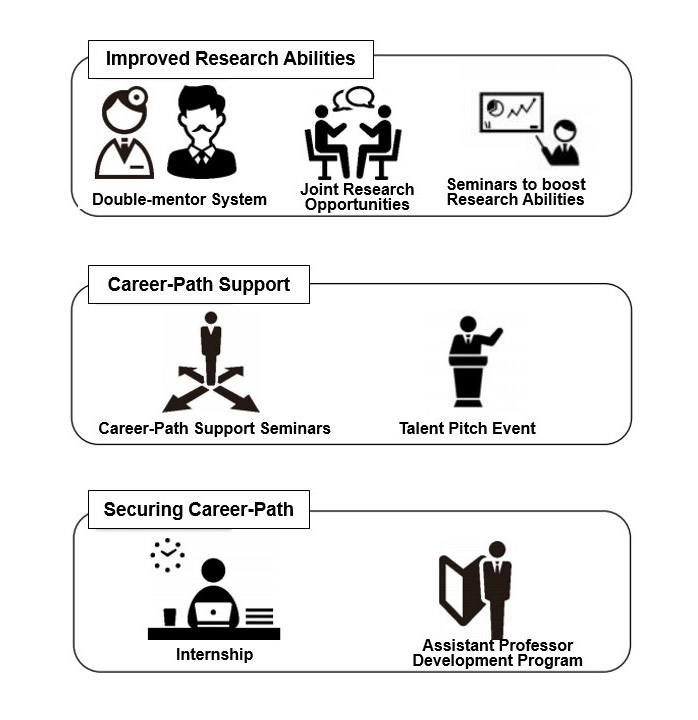
We must educate and train young individuals who can build upon the technologies we have developed and make further advancements and innovations. Chiba University has been dedicated to such education for a long time and has allocated significant resources toward this goal. For example, Chiba University’s Training Program for Information and AI Researchers to Create Innovative Medical Technologies (Research Fellowship for Informatics-based Medical Engineering: RIME) was selected in 2021 as one of the University Fellowship Program for Science and Technology Innovations by the Japan Ministry of Education, Culture, Sports, Science and Technology (MEXT). This program provides an exceptional environment for talented doctoral program students to fully engage in their research work.
Can you give us an overview of the RIME Fellowship?
One of the major pillars is economic support. In addition to the research support funding, which covers living expenses and other expenses and amounts to 170,000 yen per month, the program also grants an annual research fund of 200,000 yen. Furthermore, tuition fees are waived during the RIME-employment period. Doctoral program expenses have been a long-standing problem in Japan, and our program provides support to doctoral students from both the university and the national government.
Further, to make it easier for doctoral students to consult with experts about their research contents, we have implemented a double-mentor system, where one mentor is a medical professional and the other an engineer. Additionally, we offer a full-fledged internship system and more, which can provide practical, hands-on career selection support once the doctorate has been awarded. The RIME Fellowship program offers a solid foundation that will serve as a bridge as the doctoral student becomes a professional researcher. Our goal is to encourage more and more young researchers to contribute to our work here at Chiba University by providing the kind of support that alleviates economic issues and vague fears of the future faced by doctoral students.
Voices of RIME Program Students
Yuki Ishizaka, Doctoral Student, Graduate School of Science and Engineering
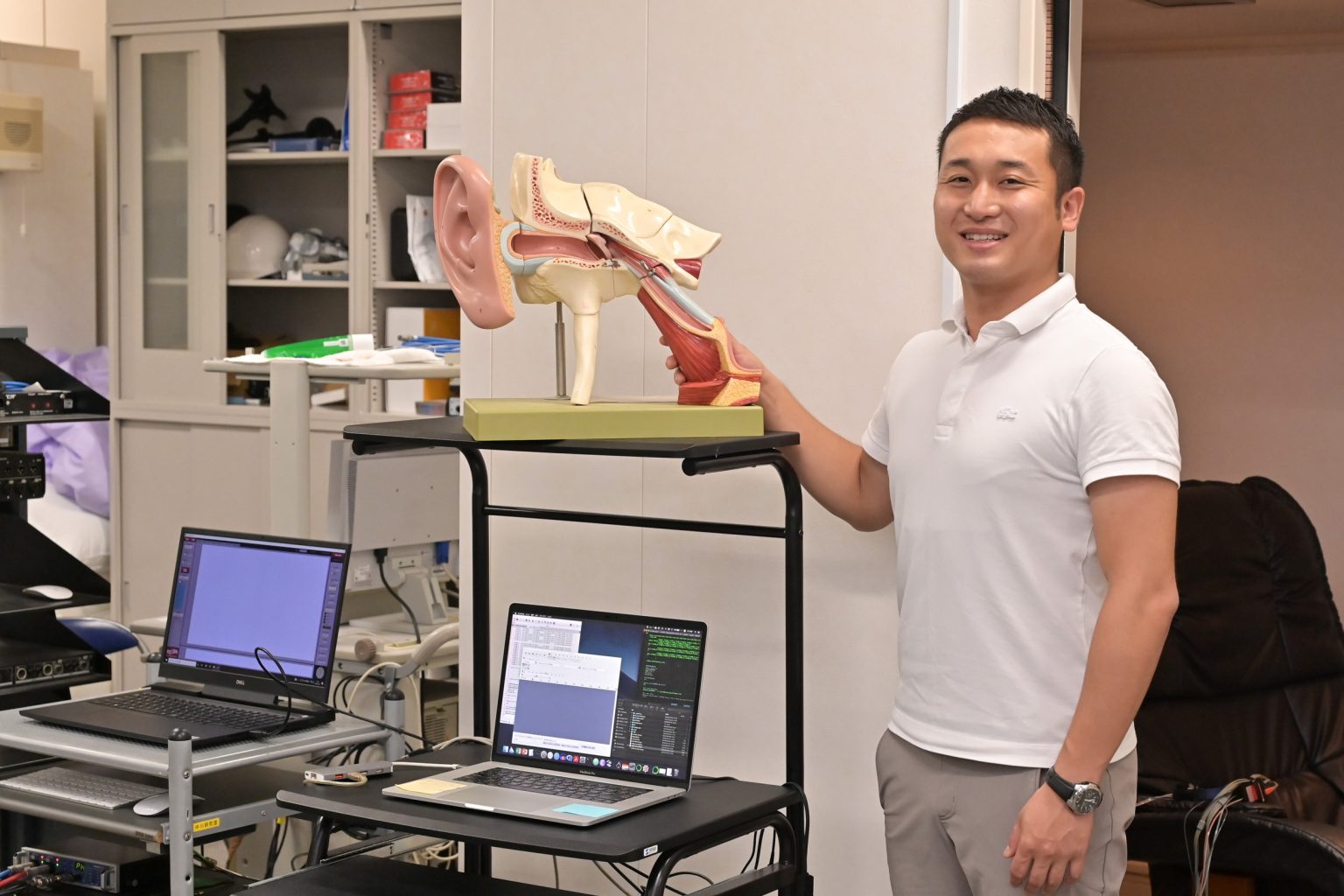
Towards a Medication-Free Solution to Noise-induced Hearing Loss for 1.1 Billion Worldwide
Prolonged acoustic overexposure causes fatigue of the sensory cells in the inner ear, resulting in impairment of hearing and speech perception. This has been termed noise-induced hearing loss (NIHL). Unfortunately, individuals with NIHL hardly notice their hearing problems until their communication is noticeably compromised since this type of hearing loss often develops slowly.
In addition, once the nerve cells are damaged, restoring them is difficult, and there are no definitive treatment options available. With an increasing number of young people listening to music through earphones or headphones, the World Health Organization (WHO) has warned that 1.1 billion people worldwide are at risk of NIHL.
Medial olivocochlear reflex (MOCR) is a protective mechanism in auditory periphery, which is thought to play an important role in protecting the inner ear from damage caused by loud noise and partly in determining the risk of NIHL. It is thought that the stronger the MOCR is, the better it can protect the ear. By strengthening the MOCR, it might be possible to alleviate NIHL without relying on drugs or other medications.
I am fortunate to have two mentors: Dr. Seiji Nakagawa of RIME, and Dr. Masato Yumoto*, a renowned expert in neuro-magnetic field measurements. I have a good relationship with both mentors and seek their guidance on topics such as cognitive functions, neuro-magnetic field measurement methods, and others. Without the support of RIME, I would not have had this fantastic opportunity.
As researchers, we are now expected to share our research findings with a wider audience, and I have been attending seminars to improve my skills in article writing and presentation. All of these experiences have been tremendously beneficial to me in my career.
*Former Director of the Epilepsy Center at The University of Tokyo Hospital, and currently Professor at Gunma Paz University.
I am fully aware of the incredible environment that has been provided for me. At the same time, this motivates me to produce results that can justify all of the wonderful benefits. My goal is to become a researcher who can showcase Japan’s research abilities to the world once again. I am grateful for the opportunity to have the time and freedom to contemplate and envision my long-term plan for the future, which is made possible by the support provided by RIME.
Yuxi Lu, Doctoral Student, Graduate School of Science and Engineering
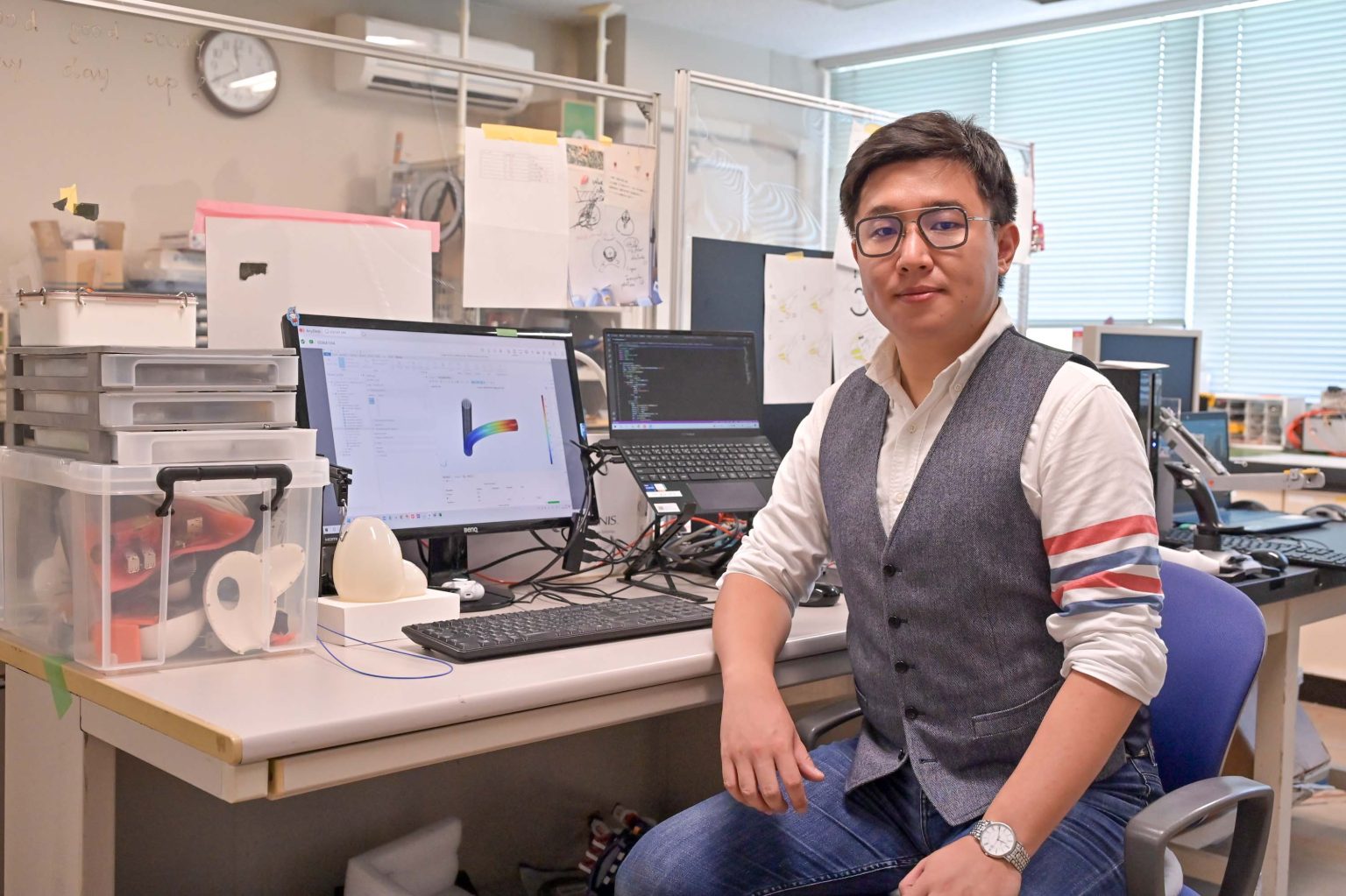
Developing a Soft Surgical Robot for Minimally Invasive Procedures to Reduce the Burden on Physicians and Patients
Upon arriving in Japan in 2013 and completing my Master’s degree at the Tokyo University of Science (TUS), I developed a keen interest in tackling medical challenges. Consequently, I joined Chiba University, a renowned institution celebrated for its numerous accomplishments in medical engineering. I focused on surface modification technologies (SMT), such as coatings and the development of optimal lubricants, to augment the functionality and applicability of materials. I believe that integrating these technologies with medical equipment and devices can substantially boost their performance. This conviction inspired me to broaden my research scope to encompass the development of user-friendly surgical robots that minimize strain on patients.
While endoscopic surgery is less invasive than open surgery, it still employs rigid surgical instruments, or actuators, which can lead to internal injuries due to the delicate and intricate nature of human tissue. Furthermore, the restricted maneuverability of these rigid instruments poses significant challenges for surgeons. Given the rising prevalence of prostatectomies, there is an escalating demand for soft-material actuators. Guided by my esteemed mentors, Pro. Wenwei Yu, a preeminent medical robot researcher, and Pro. Tatsuo Igarashi, a distinguished urology specialist, I have been granted invaluable insights into the needs and preferences of medical professionals, enabling me to progress in my R&D endeavors effectively.
My association with Chiba University stems from a resolute determination to address genuine medical predicaments. I am profoundly grateful for the support of RIME and the expert guidance of medical practitioners, which has empowered me to conduct meaningful research. Collaborating with these specialists has been an incredibly enriching and enlightening experience. Our research team actively liaises with international institutions and accommodates numerous international scholars, which has facilitated my linguistic growth, allowing me to become proficient in Chinese, Japanese, and English.
I am confident that the advancement of minimally invasive soft surgical robots will revolutionize urological and respiratory surgeries. By alleviating the pressures on doctors and patients, these robots will heighten the safety of minimally invasive procedures. Moreover, I am determined to enhance the functionality and user-friendliness of these devices to support surgeons better. I am committed to pursuing my research at Chiba University, leveraging my knowledge and experience to attain exceptional research outcomes. Simultaneously, I am eager to mentor my younger colleagues in our laboratory, channeling their creativity towards tangible research achievements, and nurturing research talent that can contribute to a more promising future for all.
Recommend
-
Exploring the uncharted waters in paleontology: Studying “Fossil Poop” as an academic survival strategy
2023.01.25
-

Creating a Flourishing Society with Novel Cultivars of Fruits: Integrating Molecular Genetics, Statistical Genetics, and Data Science for Efficient Fruit Tree Breeding
2023.09.08
-

Taking up Immunological Research against Incurable Diseases−The Significance of “1” Life
2023.01.12